Intestinal bacteria composition is crucial to driving the recovery of neutrophils counts in the blood of mice following treatments such as stem cell transplants or chemotherapy.
Kateryna Kon/Shutterstock
White blood cells, or granulocytes, are cells that are part of the innate immune system. The most common type of granulocyte is the neutrophil, a phagocyte that destroys microbes in the body. Low neutrophil counts in the blood is called neutropenia; this condition is commonly seen in cases of leukemia or following chemotherapy. It is known that neutropenia induces granulopoiesis, the process formation of granulocytes. However, the exact mechanisms by which neutropenia drives granulopoiesis are not fully understood.
A team of researchers led by Associate Professor Daigo Hashimoto and Professor Takanori Teshima at Hokkaido University’s Faculty of Medicine have discovered that the gut microbiome plays a critical role in driving granulopoiesis in mice models. Their findings were published in the journal Proceedings of the National Academy of Sciences.
The process of increasing granulopoiesis above a homeostatic level can be divided into emergency granulopoiesis, driven by the presence of bacteria, and reactive granulopoiesis, where granulopoiesis is increased in the absence of active microbial infections. It was known that reactive granulopoiesis occurs after neutropenia caused by hematopoietic stem cell transplantation (SCT) or cancer chemotherapy. The team wanted to understand the mechanisms by which neutropenia triggered reactive granulopoiesis in these two scenarios.
The team induced prolonged neutropenia in mice models, and observed the levels of cytokines, cell signalling molecules, known to be associated with granulopoiesis. They found that two cytokines were significantly elevated: the granulocyte-colony stimulating factor (G-CSF) and interleukin 17A (IL-17A). They showed that IL-17A was critical for neutrophil recovery. They confirmed that T cells are the primary source of IL-17A.
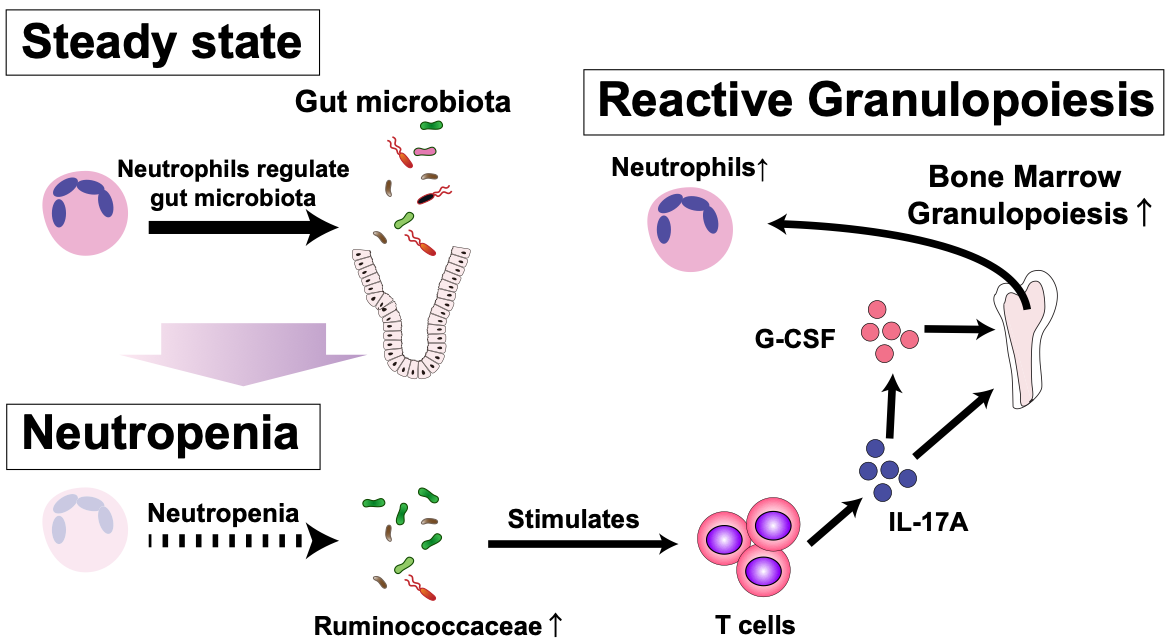
Under normal conditions (steady state) neutrophils regulate the gut microbiota. When the number of neutrophils drops (neutropenia), the composition of the gut microbiota changes, stimulating T cells to produce IL-17A. IL-17-A in turn stimulates the production of neutrophils in the bone marrow (reactive granulopoiesis). (Image: Daigo Hashimoto).
They were interested in examining if the gut microbiome influenced granulopoiesis, building on other research that suggested the gut microbiome and bone marrow haematopoiesis could affect each other. They found that the gut microbiome does upregulate reactive granulopoiesis via the IL-17A secreted by T cells, and also found that prolonged neutropenia alters the gut microbiome. They determined that it was this change in microbiome composition that enhanced reactive granulopoiesis.
This study demonstrated that the changes in intestinal microbiome induced by neutropenia stimulates reactive granulopoiesis in the bone marrow via IL-17A secreted by T cells, promoting neutrophil recovery. Future work will focus on clinical trials to test if this crosstalk is found in humans; other avenues include the development of antibiotic formulations that leave granulopoiesis-supporting bacteria intact.

Members of the Department of Hematology, including first author Xuanzhong Chen (third from left), and corresponding authors Takanori Teshima (second from left) and Daigo Hashimoto (fourth from left). (Photo: Daigo Hashimoto).
Original Article:
Xuanzhong Chen, et al. Reactive granulopoiesis depends on T-cell production of IL-17A and neutropenia-associated alteration of gut microbiota. Proceedings of the National Academy of Sciences. November 21, 2022.
DOI: 10.1073/pnas.2211230119
Funding:
This study was supported by Japan Society for the Promotion of Science KAKENHI (25293217, 20K21610, 21K08409, 21K16259, 20K17366), the Center of Innovation Program of the Japan Science and Technology Agency (JST), COI-NEXT of JST (JPMJPF2108), Promotion and Standardization of the Tenure-Track System, and Suhara Memorial Foundation.
Contacts:
Associate Professor Daigo Hashimoto
Department of Hematology
Faculty of Medicine
Hokkaido University
Email: d5hash[at]pop.med.hokudai.ac.jp
Professor Takanori Teshima
Department of Hematology
Faculty of Medicine
Hokkaido University
Email: teshima[at]med.hokudai.ac.jp
Sohail Keegan Pinto (International Public Relations Specialist)
Public Relations Division
Hokkaido University
Tel: +81-11-706-2186
Email: en-press[at]general.hokudai.ac.jp
Related Press Releases:
Loss of intestinal goblet cells causes fatal disease after stem cell transplantation
Global News and Health Forum
Comments (0)